Sleeve Gastrectomy
Overview
Originally performed as part of a more complex bariatric operation, the sleeve gastrectomy was first performed as a standalone operation in 1990. It has since increased in popularity, with gastric sleeve accounting for 61% of bariatric operations performed in the U.S. in 2020.
The sleeve gastrectomy is considered a restrictive operation, limiting the amount someone can eat comfortably. There are also hormonal changes that occur that allow the body to “let go” of excess weight.
Sleeve gastrectomy is appropriate for a wider variety of patients, including high-risk surgical patients or patients on multiple medications, since the procedure has less chance of interfering with your body’s ability to absorb oral medicines. Sleeve gastrectomy does have the risk of making gastric reflux worse.
On average, patients who choose sleeve gastrectomy lose around 65% of their excess body weight over a 12 to 18 month period.
Procedure
The gastric sleeve procedure is performed laparoscopically or robotically, with instruments passed through small incisions in the abdomen.
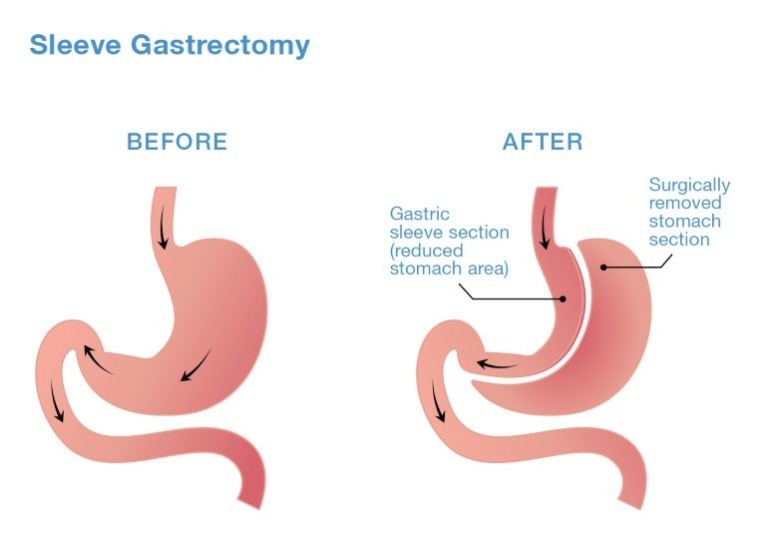
During the operation, which is performed under general anesthesia, surgeons use surgical staplers to divide the stomach and reduce the volume of the stomach by about 80%. The remaining stomach is about the size and shape of a small banana. The excess portion of the stomach is removed from the body, making the procedure non-reversible.
This new stomach sleeve can hold much less, physically limiting the amount of calories a person can consume. It also causes hormonal changes that help regulate hunger and satiety, allowing the body to lose excess weight.
The Hoag Bariatric Weight Loss Program is dedicated to providing the highest level of patient care, based on best practices that lead to quality outcomes. Meet our our bariatric team.
